How does someone develop Achilles tendon pain? To answer this question, we first have to discuss a little anatomy.
A tendon is a very thick fibrous band of tissue that connects muscle to bone. The Achilles tendon connects the two calf muscles (larger gastrocnemius and smaller soleus) to the back of your heel (calcaneus bone). It is covered by a thin sheath called the peritendon that helps it move freely against the surrounding tissues. Structurally the Achilles is similar to the patellar tendon of the knee in that every time you walk, run or jump, they both act to absorb, store and then release energy like a spring.
Every single day the tissues of your body (muscles, tendon and even bone) are in a constant process of fluctuation. Every time you place a stress on your body (like when working out) portions of your tissues are degraded and then regenerated. Overtime this natural replenishing process is how strength is built.
In your tendons, this process is largely controlled by small cells called tenocytes that are dispersed amongst aligned fibers called collagen (type 1 if you want to be exact). Tenocyte cells react to the forces and loads placed on the tendon and adapt the cellular make-up of the tissue accordingly (called the extracellular matrix). Depending on a number of factors (such as how intense you have trained throughout your years as an athlete, the medications you take, whether or not you have diabetes, etc.) your body will have adapted your Achilles tendon to a certain set point of strength called the “load tolerance” level.

Training loads placed on the tendon that do not severely exceeded this set level create a cellular response in the tendon (that can actually be seen by ultrasound) that will return to normal in 2-3 days given proper recovery methods (this is the normal time frame for the adaption “replenishment” process to take place).1 However, if the load placed on the tendon is too extreme or if there is inadequate recovery in the athlete’s training program, this balanced process is disrupted. When this occurs the process tips from being adaptive to pathological. A spark is lit and the injury process begins.

Finding Your Place On the Continuum
Before we go into how to treat tendon injuries, we first need to dive a little deeper into how the injury process occurs. The most practical way for understanding this comes from the ‘Continuum of Tendon Pathology’ by renowned expert Jill Cook.2 This model describes a continuum with three overlapping stages of injury (reactive tendinopathy, tendon disrepair and degenerative tendinopathy). Progression from one stage to the next is met with a subsequent decreasing ability to recover back to the prior healthy state.
 This model is fairly new and goes against how the medical community views chronic tendon injuries. Contrary to what your medical doctor may have told you, the term “tendinitis” isn’t technically correct (the ending “itis” refers to inflammation) as newer studies have emerged showing there is not any inflammation in affected tendons!13 For this reason the term “tendinopathy” is used as a better term to describe any tendon injury.14
This model is fairly new and goes against how the medical community views chronic tendon injuries. Contrary to what your medical doctor may have told you, the term “tendinitis” isn’t technically correct (the ending “itis” refers to inflammation) as newer studies have emerged showing there is not any inflammation in affected tendons!13 For this reason the term “tendinopathy” is used as a better term to describe any tendon injury.14
As mentioned before, when exposed to an overload of any nature there is a short term exaggerated response of the cells that make up the tendon. Specifically, small proteins called proteoglycans flood the extracellular matrix causing the tendon to become swollen and painful. Again, this swelling process is not caused by inflammation!3
This can be sparked in a few ways. The first is an acute overload of one specific or a group of training sessions that was much more intense than normal. In this scenario, the tendon experiences loads much higher than the current capacity tolerance. It can also occur upon returning to relatively “normal training” after taking an extended break from the gym (such as a week long vacation or time away due to recovering from a completely different injury). In this scenario, the time away from the gym led to an adaptive lowering of the tendons load capacity. Jumping quickly back into “normal training” caused a similar overload and sparked the exaggerated cellular response (called reactive tendinopathy). Overload can even occur through something as simple as a change in footwear (such as a shoe that provides less support, has stiff soles, or a lower heel height than your previous pair).
There is no absolute set amount of weight or reps of any drill that will automatically trigger this injury response, it comes down to purely whether or not an individual’s tendon “load capacity” has been exceeded. Elite athletes clearly have more loads placed on their tendons during their day in and day out training compared to amateurs in the same sport, yet the injury prevalence is not higher for elite athletes. The tendons of elite athletes have adapted to heavy training loads through good recovery methods combined with excellent programming/training regimes.
Now here’s the good thing, this process is reversible if properly managed. If you remove the trigger that caused the overload and allow the tendon to heal with proper rehabilitation principles (which we’ll talk about soon), the tendon will often return to it’s normal healthy self within a few weeks.
However, if the excessive load is not removed and you continue to train through the tendon pain, the injury continues to progress to the next stage of “disrepair.” In response to the continued overload more and more proteins (proteoglycans) flood the extracellular matrix drawing in water, which eventually starts to disrupt the architectural struts (collagen) that makes up the tendon. Eventually if this overload is not halted, the disorganized collagen starts to breakdown even more and die off as the injury enters the third stage (degeneration).
Unfortunately, it is very hard to distinguish whether or not a tendon is in disrepair. To make matters worse, you may not even know that your tendon has slipped into the late third stage because the degenerated part of the tendon doesn’t elicit pain.
So how do we find out which stage of injury the tendon is in?
What researchers like Jill Cook have found is that tendon pain is primarily a symptom of the “reactive” stage. For this reason, if you are currently experiencing Achilles tendon pain, you can stage your injury into an even more simple two-stage model of either “reactive” or “reactive on disrepair/degeneration” tendinopathy.2 Let me explain.
Let’s say this is the first time you’ve ever experienced Achilles tendon pain. You had a really difficult training session and the next day your Achilles hurts so bad you’re forced to limp around. Because this is an acute (brand new) episode of tendon pain, it’s likely you’re experiencing the first stage of “reactive” tendinopathy.
However, let’s say this is not the first time you’ve experienced Achilles tendon pain. You had a small flair up last year and a few months ago as well. You took a few weeks off and the pain eventually went away, but it keeps on coming back. Due to the chronic nature of these symptoms, it’s likely you may be experiencing a case of “reactive on disrepair/degeneration” tendinopathy.

When the tendon experiences continued episodes of overload, degradation can begin but the entire tendon doesn’t just die off. If you looked deep into the tendon, you’d actually notice “islands” of degenerated collagen tissue dispersed amongst healthy tendon. The small “islands” of degenerated tissue are unable to bear any load. They usually lose tensile strength and spring-like capacity which renders them “mechanically deaf” as professor Jill Cook says.
Think of the islands of degenerated Achilles tendon fibers as holes in a donut. These holes are surrounded by healthy tissue. However, research has shown the body will actually adapt and “grow” more normal tendon tissue around these dead spots in an effort to recover this lost strength.9

As mentioned before, these degenerative “holes” of the tendon do not create any pain.2 It is not until the surrounding portion of healthy tissue becomes overloaded and slips into a “reactive” phase (in the exact same way as a perfectly healthy tendon would) that pain can develop in a degenerated tendon. This is why someone could have a very degenerated tendon rupture without currently having any symptoms of pain.8
A good way to differentiate between “reactive” tendon pain and “reactive on disrepair/degeneration” (other than a history of previous symptoms) is how intense the pain is, the exact mechanism that set off the injury and how long it takes to recover. For example, a true “reactive” tendon is very painful and swollen. It is sparked by a very severe overload (running a half marathon for the first time or an extremely difficulty training session filled with a ton of plyometric exercises).
On the other hand a “reactive on disrepair/degenerated” tendon can be sparked by much less dramatic activity overload and won’t be accompanied often by as much swelling to the tendon. Pain from this particular tendinopathy can resolve in as little as a few days with proper rest, where as true “reactive” tendons can take anywhere from 4 to 8 weeks.17 Understanding which stage your symptoms present will dramatically affect how we attempt to manage the injury.
Classifications of Achilles Tendon Injuries
Overload causes tendons to spark into a “reactive” mode and become painful. Simple enough, right? Unfortunately, the Achilles tendon is a little more complicated than that. The Achilles tendon complex can become overloaded and injured in a few different ways, all which have slightly different symptoms and require different approaches to fix.3,5,10
Mid-Tendon
A mid-tendon injury is caused by an overload in tensile load (a pulling force similar to stretching out a rubber band). Your Achilles tendon acts similar to a spring when you run and perform multiple jumps. As you land, your tendon stretches under load and quickly releases power to propel your body up and away. This rapid recoil force production is called the stretch shortening cycle (SSC) and is the foundation behind plyometric training.

If the adapted tolerance set point for storage and release loads of the tendon is exceeded (due to too much volume or intensity of training) the reactive phase can be sparked. For this reason, it is common to see mid-tendon Achilles injuries in athletes who perform intense periods plyometric movements in training or competition (runners, basketball, volleyball, etc.).
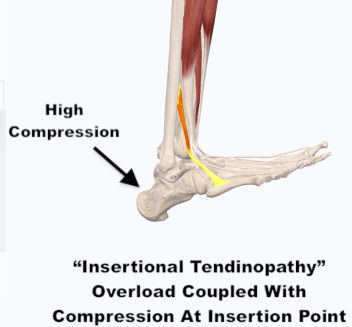
Insertional
Contrary to a mid-tendon injury, insertional tendinopathy is localized to the point where the tendon attaches to the calcaneus (heel bone). This area may be swollen and appear more pronounced upon examination. While a mid-tendon injury is believed to be largely due to an overload of tensile loads, insertional tendinopathies are largely a combination of tensile and compression.

The amount of compression placed on the Achilles tendon against calcaneus bone depends upon the position of the ankle. Activities that load the Achilles tendon but keep the ankle in a plantarflexed position (such as repetitive hopping on the toes) will not likely bring out pain. On the other hand, activities that involve loading the ankle in dorsiflexion (squatting, lunging, running up hills or on soft surfaces like on a sandy beach, or even walking barefoot) will bring out pain as the shin is pulled into a more angled position compressing the Achilles against the heel bone.11 Interestingly enough, attempts to stretch the calf muscles to relieve these symptoms will only serve to create more pain with insertional tendinopathy as the ankle is pulled into dorsiflexion, creating more compression!
Peritendon
This type of injury is not a true tendinopathy like the prior two, as the injury is not to the tendon itself but to the thin lining that surrounds it. Pain is created by constant friction of the Achilles tendon against the surrounding sheath (the peritendon) during continuous low-load ankle movement rather than overload of force like the other two issues.
For example, the peritendon can become injured during a long bike ride or after rowing a long distance. A major diagnostic sign is cracking or popping sound/sensation called crepitus that occurs as the tendon fails to move smoothly within the thickened peritendon.12 Left untreated, this injury can become very painful and disabling for an athlete.

The Assessment
The first priority during the physical examination for Achilles tendon pain is to make sure there hasn’t been a complete rupture of the tendon. An easy way to do this is with the calf squeeze test.4
Lie on your stomach with your feet freely hanging over the edge of a bed or bench. Have a friend squeeze your calf muscle and see what happens to your foot. If the foot moves when the calf is squeezed, it means the Achilles tendon is intact and we can move to the next step.
The next step is to diagnose the type of tendinopathy you are experiencing. The process is actually fairly simple. We don’t even need an expensive MRI machine. All you need to do is review how the pain started, where you’re experiencing symptoms, and then evaluate how the body responds to loading.
True Achilles tendinopathy symptoms manifests either at the insertion or in the mid-tendon and is provoked by load.7 While both are related to overload, the mechanism of overload differs between the two. Here’s how you you can test your hypothesis. During each test, grade your pain on a scale of 0-10 (zero being no pain and ten being the worst pain you could imagine).
Start with a double leg heel raise followed by a single leg heel raise while standing on flat ground. If you did not have pain, try to perform the same actions, but with your heels hanging off the side of a step or plate. This time, allow your heels to sink off the ledge as you lower yourself after performing the initial heel raise. If you had no pain on flat ground but had pain with the heel dropped version, you probably have insertional Achilles tendinopathy.
On the other hand, if you have pain with a heel raise on flat ground and your pain is located 2-7 cm above the calcaneus, you are likely dealing with mid-tendon Achilles tendinopathy. Try performing multiple jumps or hops. If this repetitive higher load motion creates more pain than a slow controlled heel raise, you can bet its mid-tendon Achilles tendinopathy. Location of pain and when the pain occurs during testing can help differentiate between mid-tendon or insertional Achilles tendinopathy.
The response to these loading tests will however be very different for someone with a peritendon injury. While someone with a mid-tendon injury will have more pain as load is increased from a slow heel raise to a faster hop, a peritendon injury may present in the complete opposite manner. A slow heel raise could cause more pain as the ankle is controlled through a larger range of motion, contributing to more friction of the peritendon.
The main take away is that diagnosing a tendinopathy doesn’t require a pricy MRI. In fact, looking at an MRI may lead your diagnosis astray as it is very common to see abnormal signs of tendon degeneration in those without any symptoms of pain!18 A doctor may be able to see you have tendon pathology by your imaging, but that alone doesn’t necessarily that is the cause of the symtpoms.
Poking and prodding around the tendon to see if it hurts is not enough to diagnose tendinopathy either. You must test the functional capacity of the tendon with load testing. If it is really a tendinopathy injury, the results of the prior tests will clearly tell you. Keep in mind that if your tendon is currently very “reactive” you may have pain with all of the prior tests regardless of whether it is insertional or mid-tendon.
Other Helpful Tests
Testing ankle mobility should always be a part of the screening process when dealing with an injury to this area of the body. When the gastroc and/or soleus muscles are stiff or short, there is less range of motion to absorb load during activities like landing from a jump. In this case, the Achilles tendon is placed under greater strain.12 Limited ankle mobility can be a risk factor for mid-tendon Achilles tendinopathy because the tendon will have less range to absorb load therefore the tendon has to take more load more quickly.17 With insertional Achilles tendinopathy, less dorsiflexion may place less compression on the insertion. Therefore, poor dorsiflexion mobility is more of a risk factor for mid-tendon and not insertional.
The 5 inch wall test is a very simple screen you can perform on your own.15,16 Kneel down by a wall and place your toes five inches from its base. Drive your knee straight forward over your toes attempting to touch the wall without letting your heel pop off the ground.
What did you find?
Were you able to touch the wall with your knee, or did your heel pull off the ground? If you failed the 5-inch wall test, you just uncovered a weak link in ankle mobility that needs to be addressed.
Although not supported by strong research, these are other factors that may influence Achilles tendinopathy:
- Biomechanical dysfunction
- Poor double leg or single squat
- Poor jumping/landing mechanics
- Poor/inefficient Running mechanics (forefoot striker or low steps per minute)
- Weak hip muscles (glute max and glute medius)
Final Thoughts
Achilles tendon pain is no simple injury. The tendon complex is engineered to absorb high level of loads and will adapt over time and become stronger if trained appropriately. However, this adaption process is slow and overload can easily occur with athletes in almost any sport.
Understanding the key concepts of how this injury starts and progresses will empower you to better manage the symptoms and return to the sports and activities you love. Next week we’ll go over just how to start fixing your Achilles tendon pain.
Until then,

With

Want To Attend A Squat University Seminar!?
Upcoming Dates
April 13-14: Ireland (Register here now!)
**Thank you to 3d4Medical.com with the Complete Anatomy app for the visuals of the body today!**
References
- Rosengarten SD, Cook JL, Bryant AL, et al. Australian football players’ Achilles tendons respond to game loads within 2 days: an ultrasound tissue characterization (UTC) study. Br J Sports Med. 2015;49:183-7
- Cook JL, Rio E, Purdam CR, Docking SI. Revisiting the continuum model of tendon pathology: what is its merit in clinical practice and research? Br J Sports Med. 2016; 50(19):1187-1191
- Alfredson H, Cook J. A treatment algorithm for managing Achilles tendinopathy: new treatment options. BJS
- Maffulli N. The clinical diagnosis of subcutaneous tear of the Achilles tendon. A prospective study in 174 patients. Am J Sports Med. 1998;26:266-70
- Cook JL, Stasinopoulos D, Brismée JM. Insertional and mid-substance Achilles tendinopathies: eccentric training is not for everyone – updated evidence of non-surgical management. Journal of Manual & Manipulative Therapy. 2018;26(3):119-122
- Ganderton C, Cook J, Docking S, Rio E, et al. Achilles tendinopathy: understanding the key concepts to improve clinical management. Australasian Musculoskeletal Medicine. 2015;19(2):12-18
- Kountouris A, Cook J. Rehabilitation of Achilles and patellar tendinopathies. Best Pract Res Clin Rheumatol. 2007;21:295-316
- Rio EK, Ellis RF, Henry JM, Falconer VR, et al. Don’t assume the control group is normal – people with asymptomatic tendon pathology have higher pressure pain thresholds. Pain Medicine, 2018;0(0):1-7
- Docking SI, Girdwood MA, Cook J, Fortington LV, Rio E. Reduced levels of aligned fibrillar structure are not associated with Achilles and patellar tendon symptoms. Clin J Sport Med. 2018.
- Docking SI, Ooi CC, Connell D. Tendinopathy: is imaging telling us the entire story? J Orthop Sports Phys Ther. 2015;45(11):842-52
- Cook JL, Purdam C. Is compressive load a factor in the development of tendinopathy? Br J Sports Med. 2011;1-6
- Reynolds NL, Worrell TW. Chronic Achilles peritendinitis: etiology, pathophysiology, and treatment. JOSPT. 1991;13(4):171-176
- Khan KM, Cook JL, Kannus P, Maffulli N, Bonar SF. Time to abandon the “tendinitis” myth: Painful, overuse tendon conditions have non-inflammatory pathology. BMJ. 2002;16:324(7338):626-627
- Maffulli N, Khan KM, Puddu G. Overuse tendon conditions: time to change a confusing terminology. Arthroscopy. 1998;14(8):840-3
- Bennell K, Talbot R, Wajswelner H, Techovanich W, Kelly D. Intra-rater and inter-rater reliability of a weight-bearing lunge measure of ankle dorsiflexion. Australian Journal of Physiotherapy. 1998; 44(3):175-180.
- Reinold M. (2013) Ankle mobility exercises to improve dorsiflexion. Retrieved from MikeReinold.com.
- Cook J. (2018, November 5). Personal Communication.
- Docking SI, Rio E, Cook J, Carey D, Fortington L. Quantification of achilles and patellar tendon structure on imaging does not enhance ability to predict self-reported symptoms beyond grey-scale ultrasound and previous history. J Sci Med Sport. 2018;S1440-2440(18)30420-1
Big thanks to 3d4Medical and their app Complete Anatomy for the visual of the body today. If you would like to use their app at a discounted price, check out this link: https://store.3d4medical.com/application/user-kind?id=1&promo=uRSj7I7YOr








Hi, I believe I have insertional Achilles tendinopathy.
What are some strengthening exercises I can do for this?
Thank you so much for sharing all you knowledge
[…] back to Squat University. Last month I started a blog series on the topic of Achilles tendinopathy. The first blog introduced a simple model to better understand why the injury process begins and […]
If each test is to see what triggers pain by those movements, how do you decipher which ankle injury you are likely to have if you are currently experiencing pain at rest with the achilles tendon? Currently just standing and walking causes immediate pain in my ankles. Dealing with pain in both ankles, and both knees for 6 months.
Exactly, these are the reasons which cause Tendon Pain and if a person could manage to avoid these things, he can prevent Tendon Pain. I read the article meticulously so that I can read about these things which can cause me sever tendon pain. Definitely I will do suggested exercise to prevent this pain. Well, I always visit EduBirdie source to read reviews of the people about writer before hiring him to write me an essay on topics like this.
PT, DPT, CSCS, USAW
Think I’ll go elsewhere
Where does pain in the musculotendinous junction fit in to this continuum?
Thanks, squatuniversity, great as always!
When choosing a moving company for a long-distance move, look for a company with experience and expertise in the type of move you’re making. Mowers Shipping Cost
I’ve had pretty bad achilles pain while running/hiking but never in a gym. Switched to ankle support boots from nearby outdoor/sports store and it’s fine again. I know it’s probably a stability issue, but helps short term(probably gotta adress it at some point).
Just performing system administration tasks using Pubnix Online https://pubnix.com/. I communicate via email with clients and coworkers, and the file-sharing feature makes it simpler to work together on projects. By utilizing the Unix Scripting Toolkit to automate administrative tasks, I have saved time and effort. The platform offers excellent support and readily available documentation. recommended for everyone. I recommended everyone.
Exercising properly at the gym will help mr mine quickly get the body shape we dream of and help our muscles move more flexibly.
Thanks for providing very detailed information on how Achilles tendon pain develops. It helped me understand my body and how to structure my training program to avoid injury. By the way, if you have difficulty calculating your working hours or salary, time calculator is the perfect suggestion to help you solve that problem.
When it comes to BC Game https://bcgame.fr/ online, all I do is run administrative chores. With the file sharing function, I can easily collaborate on projects with customers and coworkers, and I can connect with them via email. Automating administrative activities using the Unix Scripting Toolkit has helped me save a lot of time. The platform provides top-notch support and documentation is easy to find. suggested for all individuals. I would suggest it to everybody.
Could you recommend any workouts that might help me strengthen this area doodle jump ?
Ethical considerations come into play concerning the privacy and consent of individuals depicted by tifa sexdolls, If the creation or distribution of these tifa sexdoll s involves unauthorized use of someone’s likeness or violates their privacy rights, it could lead to legal consequences such as defamation or invasion of privacy claims.
Good !!
Whether you’re making simple choices or need to resolve a complex decision, using a tool like a picker wheel can help you make quick and effective choices. Visit this website to get access to picker wheel: https://yesornowheel.cc/. It’s a great way to bring a fun and easy solution to decision-making processes.
I appreciate platforms that keep things simple, and this one nails it. There’s no unnecessary clutter, just the tools and features you actually need. It’s also well-organized, which makes finding things a breeze. If you’re curious, check out this link: https://1win.com/ It might save you time and effort like it did for me.
J’apprécie la clarté de vos explications et la pertinence de vos conseils ! Je compte bien suivre vos recommandations lors de mes paris sur le soccer, le rugby et les compétitions de Fortnite https://melbet-afro.com/fr/melbet-inscription-connexion-pour-les-parieurs-africains/. Merci pour ce contenu enrichissant et accessible à tous.
We stand out by aspiring beyond the conventional, offering users not just sexual satisfaction but an entirely new dimension of experience. XSPACECUP’s mission is to guide users on an exciting, innovative, and satisfying journey of personal solo pleasure.
https://www.xspacecup.com/
We stand out by aspiring beyond the conventional, offering users not just sexual satisfaction but an entirely new dimension of experience. XSPACECUP’s mission is to guide users on an exciting, innovative, and satisfying journey of personal solo pleasure.
https://www.xspacecup.com/
The article is very detailed. Even you are interesting sports, you should read it to know how to protect your health.
That’s a great anatomical overview! Understanding the structure is key. What specific factors or activities contribute to the inflammation or degradation of this tendon and its sheath, leading to the pain you described? It’s something easily forgotten during a round of the Dinosaur Game.
This was really informative—Achilles tendon pain is something even gamers and sim racers can experience after long sessions at the rig. Staying aware of body posture and taking breaks really helps. If you’re into high-intensity car racing games like I am, you might enjoy what we’ve built: https://carxstreethd.com – it’s all about speed, strategy, and immersive racing experiences!
This was such an insightful breakdown of how Achilles tendon pain develops and why proper load management is so important for recovery. I especially liked how you explained the difference between reactive and degenerative stages—it makes it easier to understand why rest and smart training are key. For anyone dealing with recurring sports injuries or needing to manage their health better, it reminds me of how helpful online platforms like the MI Fone portal website can be for teachers and employees in tracking their official records and staying organized, just like athletes need to keep track of their training loads and recovery. Both highlight how structured monitoring can prevent bigger problems down the road.
Choosing the right SEO analyst Pakistan is the first step towards online dominance. Our SEO experts focus on building strong digital foundations that bring lasting results. Whether you want to target local customers in Pakistan or expand globally, our tailored strategies help you climb search rankings, attract organic traffic, and achieve business growth.
Your body’s tissues constantly rebuild after stress. Overdoing it in training disrupts this balance, leading to injury. The Continuum of Tendon Pathology explains this progression, moving from reactive to degenerative stages. Remember, tendinopathy is more accurate than tendinitis. Overload, even from new shoes, can trigger problems. Listen to your body and recover well. For a mental break after training, maybe unwind with some fast-paced io games online.
If each test is to see what triggers pain by those movements, how do you decipher which ankle injury you are likely to have if you are currently experiencing pain at rest with the achilles tendon? Currently just standing and walking causes immediate pain in my ankles. Dealing with pain in both ankles, and both knees for 6 months. For enjoy download https://carxstreetsapp.com/
verde casino app provides a lightweight and intuitive way for players to enjoy gambling on the go. It features stable performance and a responsive design, making it easy to have a full gaming session on your phone. You can download the app for free as an APK or use the QR code for iOS devices with version 12.0 and above. Our experts confirm that the latest version offers a trustworthy experience with fast payments, quick game loading, and quality support.
This was really informative—Achilles tendon pain is something even gamers and sim racers can experience after long sessions at the rig. Staying aware of body posture and taking breaks really helps. If you’re into high-intensity car racing games like I am, you might enjoy what we’ve built i.e carexstreetapk.com